Food Allergy
CLASSIFICATION & DEFINITIONS
ATOPY is defined as IgE sensitization as documented by IgE antibodies in serum or with positive skin prick tests (SPT)
HYPERSENSITIVITY is defined as conditions that are similar to allergy and produce reproducible signs and symptoms when exposed to offending agents or food at a dose tolerated by normal persons and caused mostly by non-immune mechanisms.
ALLERGY is defined as a hypersensitivity reaction caused by immunological mechanisms.
Based on these definitions, correct diagnosis of allergy must be supported with:-
a) Compatible clinical history; and
b) Positive SKIN PRICK TESTS, TOTAL IgE, if possible SPECIFIC IgE, and other relevant tests
IMMUNE MECHANISMS OF ALLERGY: -
1. The IgE-mediated reactions are usually divided into immediate-onset reactions (arising up to 2 hours from the food ingestion) and immediate plus late-phase (in which the immediate onset symptoms are followed by prolonged or ongoing symptoms).
2. Non-IgE-mediated reactions, which are poorly defined both clinically and scientifically, are believed to be generally T-cell-mediated. They are typically delayed in onset, and occur 4 to 28 hours after ingestion of the offending food(s).
3. Mixed IgE and non-IgE mediated reactions are conditions associated with food allergy involving both IgE- and non-IgE-mediated mechanisms3.
FOOD REACTIONS which appear to be allergic food reactions are not food reactions4 and should be called as FOOD INTOLERANCES5 and should not be termed as allergic reactions eg. lactose and alcohol intolerance, responses to pharmacologically active food components, as caffeine, theobromine in chocolate or tyramine in fermented cheeses, or toxic reactions. TOXIC REACTIONS to food can occur in any patient if a sufficient amount of the food is ingested; they are due to toxins in the food, e.g., to histamine in scombroid fish or bacterial toxins in food. Host factors such as lactase deficiency, which are associated with lactose intolerance, or idiosyncratic responses may be responsible for other non-allergic reactions to foods.
Mechanisms of Food Allergy
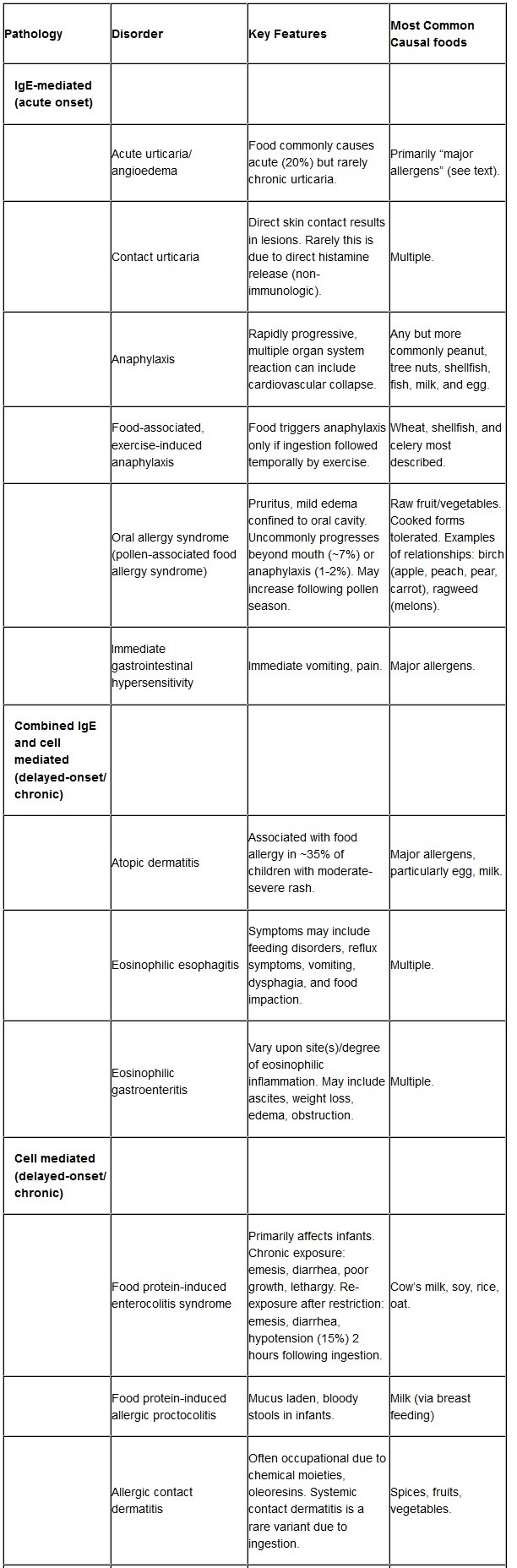
Typical food allergies are IgE-mediated, but several reactions involve different immunologic mechanisms. These food allergies are defined as non–IgE-mediated or mixed IgE- and non–IgE-mediated.
The symptoms of IgE-mediated, non-IgE–mediated, and mixed IgE- and non–IgE-mediated food allergy are presented in Table 1. IgE-mediated symptoms develop within minutes to 1-2 hours of ingesting the food, non–IgE-mediated and mixed IgE- and non–IgE-mediated food allergies present with their symptoms several hours after the ingestion of the food. These symptoms develop due to environmental, genetic factors and failure to develop tolerance to foods and result in excessive production of IgE antibodies.
Cross-Reactivity and Food Allergens
Those persons having allergy to pollens can have an allergy to certain foods due to sharing of allergens both in foods and pollens eg oral allergy syndrome (OAS), exercise induced asthma, and anaphylaxis when eating certain foods. The allergens commonly shared by pollens and foods are (PR), profilins, or lipid transfer proteins (LTP). These proteins are ubiquitous in pollens, plants, fruits, and food. Individuals sensitive to house dust mites have been reported with oral allergy syndrome following ingestion of shellfish13. Children with CMA may react to beef in up to 20% of cases, to goat’s milk in 98%, 14.
CROSS REACTIVITY OF GRASS POLLEN & FOODS:-
Persons having asthma or sneezing, watering nose, headache and watering itching eyes and have allergy due to grass pollen will have same symptoms when they eat tomatoes, peanut, pea, wheat, rye, peach, water melon, orange and potatoes or vice versa if someone is allergic to these foods and have signs and symptoms of Oral Allergy Syndrome (itching and redness around the mouth, swelling and itching of mouth), gas abdomen, pain abdomen, loose stools, heartburn, dizziness, itching on body, rashes, eczema, fatigue and tiredness, memory and concentration problems, irritability, aggressiveness, behavioral disorders, depression anxiety etc they will develop these symptoms even on exposure to the Grass pollens.
CROSS REACTIVITY OF RAGWEED & MELON, BANANA
CROSS REACTIVITY OF CANNABIS POLLEN TO TOMATO, PEACH AND HAZELNUT
CROSS REACTIONS OF HOUSE DUST MITE ALLERGIC PATIENTS TO SEAFOODS LIKE SHIRMPS, CRABS, LOBSERS
CROSS REACTIVITY OF LATEX & BANANA, CHESTNUT, KIVI, AVACADO
CROSS REACTIVITY OF BIRCH POLLEN & NUTS, APPLE, PEAR, PEACH, PLUM, CHERRY, CARROT, PEANUT, SOYA
IgE-Mediated Food-Related Disorders
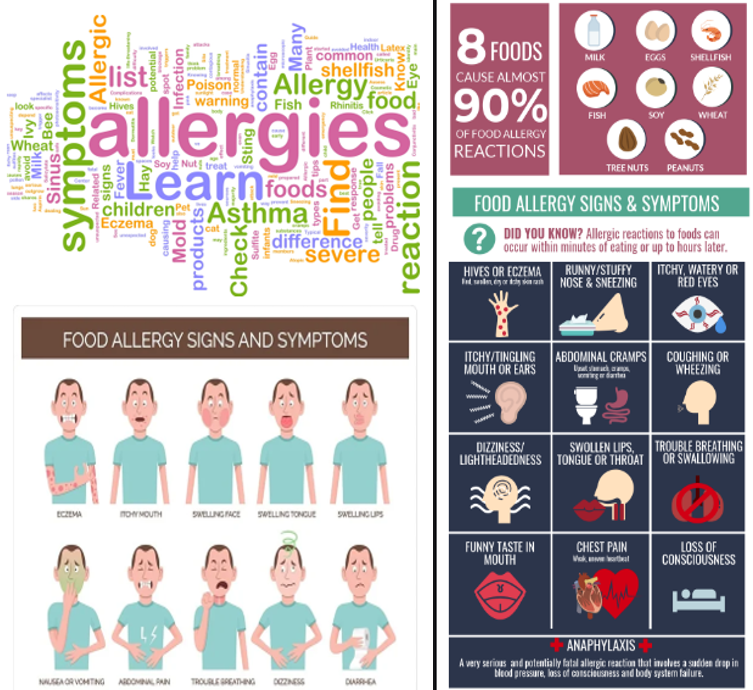
Skin Manifestations (Urticaria Angoedema)
Acute urticaria and angioedema are the most frequent manifestation of food allergy. The onset of symptoms may be rapid, within minutes, following the ingestion of the offending food. Foods most often implicated include milk, fish, vegetables, and fruits. In atopic dermatitis, also a frequent symptom of food allergy, immediate reactions can be followed by late cutaneous reactions.
Gastrointestinal Tract
Symptoms caused by immediate sensitivity in the gastrointestinal tract typically develop within minutes to 2 hours of ingesting the offending food. Symptoms can include lip, tongue, and palatal pruritus and swelling, laryngeal edema, nausea, abdominal cramping, vomiting, and diarrhea. Severe reactions can result in most or all symptoms associated with anaphylaxis.
Oral allergy syndrome (OAS)
A form of contact urticaria confined to the lips and oropharynx, most commonly occurs in pollen-allergic patients. Symptoms include oropharyngeal itching, with or without facial angioedema, and/or tingling of the lips, tongue, palate, and throat.
Respiratory Reactions
Allergic rhinoconjunctivitis and asthma can occur following food challenge testing, but respiratory symptoms from food allergy in the absence of skin or gastrointestinal manifestations are rare. When respiratory symptoms occur following food challenge, both early- and late-phase IgE-mediated mechanisms are probably involved.
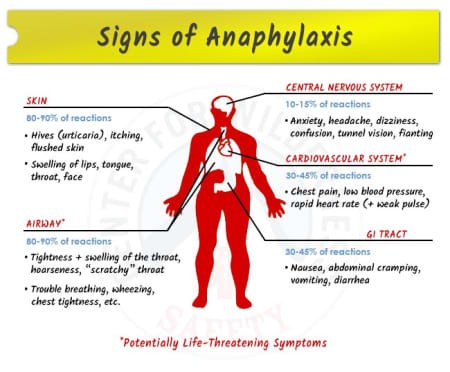
Systemic reaction: Anaphylaxis
Gastrointestinal
Food allergy is also linked to manifestations of delayed hypersensitivity, partially IgE-mediated and partially non-IgE-mediated. It is implicated in Eosinophilic Esophagitis, Eosinophilic gastritis and gastroenteritis, food protein-induced enterocolitis syndrome, and allergic proctocolitis.
Food protein-induced enterocolitis syndrome (FPIES)
Primarily affects infants. In chronic forms, it presents as emesis, diarrhea, poor growth, and, in severe cases, starvation and lethargy. In acute forms, or after re-administration of restricted foods, it may determine emesis, diarrhea, and hypotension, starting two hours following ingestion. Diarrhea may be bloody and may result in dehydration, especially in early infancy. It has been associated frequently with the ingestion of cow’s milk, soy, oat, wheat, and/or rice. Skin prick tests to the suspected foods are generally negative, but IgE-mediated food allergy may be associated with FPIES as sometimes the two conditions co-exist or one form transforms into another. International consensus guidelines have been developed for FPIES.15
Food protein-induced allergic proctocolitis (FPIAP)
FPIAP is a benign transient condition, typically starting in the first few months of life with bloody stools in well-appearing infants. About 60% of cases occur in breast-fed babies, the remainder in infants fed cow’s milk or soy protein-based formulas.
Rarely, dietary protein proctitis shows mild hypoalbuminemia and peripheral eosinophilia. Bowel lesions are usually confined to the distal large bowel; endoscopy reveals linear erosions and mucosal edema with infiltration of eosinophils in the epithelium and lamina propria.
Food-induced pulmonary haemosiderosis (Heiner’s Syndrome)
This very rare syndrome, affecting infants and young children, is characterized by recurrent episodes of pneumonia associated with pulmonary infiltrates, hemosiderosis, gastrointestinal blood loss, iron deficiency, anemia, failure to thrive. It is due to cow’s milk16; the immunologic mechanism is still unknown.
Mixed IgE and non-IgE reactions
Eczema
Although it is not, strictly speaking, an allergic disease, at least one-third of infants and young children with atopic eczema have IgE-mediated food allergies. Egg allergy is the most common food hypersensitivity in children with eczema. Appropriate diagnosis of food allergy and elimination of the offending allergen leads to significant clearing or improvement of eczematous lesions in many young children with eczema and food allergy. Food allergens may be triggers for some acute exacerbations17.
Allergic eosinophilic oesophagitis (EoE).
This condition may present in children with a variety of nonspecific symptoms, e.g., feeding difficulty, nausea, vomiting, heartburn, and failure to thrive. Teenagers and adults are more likely to present with dysphagia and episodes of food impaction.
Eighty percent of patients with eosinophilic esophagitis have symptoms similar to gastroesophageal reflux, which are refractory to anti-reflux therapy. In the case of infants, vomitus often contains stringy mucus (similar to egg albumin). Patients may also present with food refusal, dysphagia, food impaction, or abdominal pain. Food-induced IgE-mediated allergy has been implicated in the pathogenesis in some patients. In eosinophilic esophagitis, there may be years of unrecognized childhood subclinical disease or “silent” chronic inflammation before the diagnosis is made18.
Allergic eosinophilic gastritis or gastroenteritis
The exact cause of these disorders remains unknown although both IgE-mediated and T-cell-mediated reactions have been implicated. These conditions are characterized by infiltration of eosinophils in the mucosal, muscular, and/or serosal layers of the stomach or small intestines. Patients present with postprandial nausea and vomiting, abdominal pain, diarrhea (occasionally steatorrhea) and weight loss in adults, and failure to thrive in young infants.
Diagnosis of Food Allergy
The results of skin prick tests (SPT), IgE total and specific antibodies, and patient histories are not predictive of true food allergy, as they are not able to establish the causal and temporal relationship between the intake of the suspect food and the hypersensitivity reaction. The negative predictive accuracy of a skin prick test weal of < 3mm greater than the negative control is high, usually > 95%, and is strong evidence that the food may be consumed without severe, immediate food-allergic reactions. A positive SPT, even a weal of 3 mm or more, maybe clinically irrelevant, as the patient may tolerate the ingested food. SPTs may also remain positive after the development of tolerance to the specific food.
Specific IgE levels using the most popular diagnostic systems, it is conventionally accepted that 0.35 kU/l is the cut-off level for a positive in-vitro test of specific IgE. Higher levels of specific IgE for food allergens may better correlate with clinical reactivity as evidenced by challenge testing. We normally correlate with Intra Dermal Challenge Test and we get better results.
A double-blind, placebo-controlled food challenge (DBPCFC) is the preferred test to diagnose food allergy3,19 or we can do DFCT (deliberate food Challenge Tests)
Total IgE and specific IgE can help to identify cross-reactive allergens between pollen and foods, or foods and latex. Cross-reactive allergens include common lipid transfer proteins (LTPs), PR molecules, and profilin. Skin prick tests are often negative, but a positive test may be obtained using a drop of fresh juice from the fruit and doing the skin prick tests.
Atopy Patch Test (APT) is a skin test in which allergens commonly associated with IgE reactions can be used, although patch testing is more commonly performed for metals such as nickel, which causes a positive patch test in nickel sensitive subjects. A positive APT can predict a late phase reaction following oral food challenge. A positive APT may detect the cause of Eczema or Gastrointestinal Reactions in infants and children19. This test is not useful for IgE-mediated food allergy. It is considered experimental in most parts of the world20.
Prevention of food allergy
According to all the current guidelines, an infant with at least one first-degree relative (parent or sibling) with a history of allergic disease21,22’ in particular allergic rhinitis, asthma, eczema, or food allergy23,24 is at greater risk for developing a food allergy.
The first proposed recommendation for large-scale prevention of food allergy has been the use of hypoallergenic25 (HA) formulae in case of breastfeeding failure but this view was questioned in later research26,27,28. Emerging evidence, however, has led to a paradigm shift, supporting nutritional approaches such as appropriate timing of food exposure, and the use of prebiotics and probiotics for allergy prevention. National Institutes of Health (NIH) Guidelines for the Management and Prevention of Food Allergy subsequently recommended the introduction of peanut-containing foods to “high-risk” infants early in life (4-11 months)29. The World Allergy Organization (WAO)/McMaster Working Group Guidelines for Allergic Disease Prevention (GLAD-P) suggested using probiotics in pregnant and breastfeeding women whose children and infants are at high risk for developing allergy29 reducing allergic eczema.
Treatment
Food Allergen Avoidance
The foods to which an individual is allergic should be avoided, as therapeutic intervention (tertiary prevention) in patients with food allergy. Avoidance measures need to be tailored to the individual’s life and disease requirements must take into account the needs of growth, the prevention of anaphylaxis and, of the benefits expected of allergen avoidance itself. It is important to note that physician while considering avoidance of foods must be 100% sure of food allergy and then guide about the avoidance and he must consider the importance of unnecessary avoiding long list of foods which can have a serious effect on the nutrition of the patient and on the immune system. He must balance the AVOIDANCE AND IMMUNO NUTRITION.
From the patient’s perspective, avoidance means meeting obstacles unshared by their non-allergic peers, thereby curtailing their quality of life.
From the physician’s outlook, education, ensuring compliance, and receptiveness of both patient and caregiver are major concerns.
The role of the allergist is to review in a dialectical assessment these competing factors in concert with all parties concerned. Where avoidance of the implicated food may result in nutritional deficiency, dietary supplementation is necessary.
ALLERGY AND ASTHMA PROTOCOL FOR MANAGEMENT OF FOOD ALLERGIES: -
I am practicing Oral Allergy Immunotherapy since 2002 when it was strongly recommended that allergy tests for food allergies should not be done and no allergy immunotherapy is effective for food allergies, but I was getting very encouraging results with allergy tests and with oral allergy vaccines of Immunotherapy. Now there is a paradigm shift and all the international allergy organizations agree that allergy tests and oral allergy vaccines are effective for food allergies. Even the most severe and dangerous to manage PEANUT ALLERGY is not recommended to be treated with SLIT (Sublingual Allergy Immunotherapy) or Oral Allergy Vaccines.
• Skin Prick Tests are initial tests for the foods and if SPT not diagnostic then we do Intra Dermal Challenge tests (for persons having low to moderate allergies) or Oral Deliberate Food Challenge Tests (DFCT)
• Specific IgE Tests for 330 allergens
• Total IgE Tests
• Based on the HISTORY and results of the SKIN ALLERGY TESTS, IgE(Total & Specific), SLIT vaccine (SubLingual Allergy Immunotherapy is recommended)
• Recommended ¾ Day Rotatory Diversified Program is recommended
Processed foods may contain hidden proteins, e.g., milk, egg and soy proteins may be added to increase the protein content or enhance flavor. Peanuts and nut products are added to thicken and flavor sauces. Patients can be taught to identify hidden food components in processed foods. Hidden and possible causes of food allergies and intolerances are casein and lactose, derived from milk, and albumin from egg and 12 food items are required by law to appear on the label: cereals containing gluten, crustaceans, egg, fish, peanut, soy, milk (including lactose), tree nuts, mustard, sesame seeds, celery, and sulfites >10 mg/kg30.
Pharmacological therapy
Hypersensitivity reactions are often treated with medications. Epinephrine is the only medication that is effective for the treatment of anaphylaxis. Other medicines which are only symptomatic treatment include H1 and H2 antihistamines, corticosteroids, and prostaglandin synthetase inhibitors and are not recommended. Anti-IgE monoclonal antibodies therapy is licensed for use in asthma and chronic urticaria in many countries and may be used in the management of serious food allergies.
Oral Immunotherapy
Oral Immunotherapy is now accepted for food allergies31.
One of the most often asked parents’ questions is “How long will my child’s food allergy last?” It depends on certain factors:-
• The more severe the reaction, the less likely that the food allergy will be outgrown.
• IgE antibody level and age at diagnosis, have also been associated with prognosis of food allergy,
• Milk allergy’s half-life is approximately two years while egg allergy’s half-life is approximately four years. Peanut allergy, once considered to be a life-long condition, can resolve in up to 30% of cases32. Similarly, fish allergy is considered a long-lasting condition and reports of recovery are rare33. In food-allergic children, tolerance must be tested by an oral challenge at regular intervals. Often tolerance is not acquired suddenly, but there is a gradual increase of the doses tolerated at a challenge. Epinephrine is the only medication that is effective for the treatment of anaphylaxis34.
References:-
1. Johansson SG, Bieber T, Dahl R, et al: Revised nomenclature for allergy for global use: report of the Nomenclature Review Committee of the World Allergy Organization. J Allergy Clin Immunol 2004, 113:832–6
2. Demoly P, Tanno LK, Akdis CA, Lau S, et al. Global classification and coding of hypersensitivity diseases – An EAACI – WAO survey, strategic paper and review. Allergy 2014, 69:559–70
3. Burks AW, Tang M, Sicherer S, et al. ICON: Food allergy. J Allergy Clin Immunol 2012, 129:906-20
4. Boyce JA, Assa’ad A, Burks AW, Jones SM, Sampson HA, Wood RA, et al. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J. Allergy Clin Immunol 2010;126(6 Suppl):S1–58.
5. Dreborg S. Debates in allergy medicine: food intolerance does not exist. World Allergy Organ J. 2015 Dec 14;8:37
6.Koplin JJ, Osborne NJ, Wake M, et all. Can early introduction of egg prevent egg allergy in infants? A population-based study. J Allergy Clin Immunol. 2010;126:807-13
7. Thalayasingam M, Lee BW. Fish and shellfish allergy. Chem Immunol Allergy 2015;101:152-61
8. Sicherer SH, Muñoz-Furlong A, Sampson HA. Prevalence of seafood allergy in the United States determined by a random telephone survey. J Allergy Clin Immunol 2004;114:159-65
9. Kattan J. The Prevalence and Natural History of Food Allergy. Curr Allergy Asthma Rep. 2016;16:47
10. Xepapadaki P, Fiocchi A, Grabenhenrich L et al. Incidence and natural history of hen’s egg allergy in the first 2 years of life – the EuroPrevall birth cohort study. Allergy. 2016;71:350-7
11. Koplin JJ, Osborne NJ, Wake M, et all. Can early introduction of egg prevent egg allergy in infants? A population-based study. J Allergy Clin Immunol. 2010;126:807-13
12. Simons FE, Ebisawa M, Sanchez-Borges M, et al. 2015 update of the evidence base: World Allergy Organization anaphylaxis guidelines. World Allergy Organ J. 2015 Oct 28;8:32
13. Matricardi PM, Kleine-Tebbe J, Hoffmann HJ. EAACI Molecular Allergology User’s Guide. Pediatr Allergy Immunol 2016 May;27 Suppl 23:1-250
14. Warren CM, Jhaveri S, Warrier MR, Smith B, Gupta RS. The epidemiology of milk allergy in US children. Ann Allergy Asthma Immunol 2013;110:370-4
15. Nowak-Węgrzyn A, Chehade M, Groetch M, et al. International Consensus Guidelines for the Diagnosis and Management of Food Protein-Induced Enterocolitis Syndrome: Workgroup Report of the Adverse Reactions to Foods Committee, American Academy of Allergy, Asthma, and Immunology. J Allergy Clin Immunol. 2017 Feb 3 [Epub ahead of print]
16. Fiocchi A, Brozek J, Schunemann HJ, Bahna SL, von Berg A, Beyer K, et al. World Allergy Organization (WAO) Diagnosis and Rationale for Action against Cow’s Milk Allergy (DRACMA) Guidelines. WAO Journal 2010; 3:57-61
17. Roerdink EM, Flokstra-de Blok BM, Blok JL, ET AL. Association of food allergy and atopic dermatitis exacerbations. Ann Allergy Asthma Immunol. 2016;116:334-8
18 . Furuta GT, Katzka DA. Eosinophilic Esophagitis. N Engl J Med 2015;373:1640-8.
19. Boonyaviwat O, Pacharn P, Jirapongsananuruk O, Vichyanond P, Visitsunthorn N. Role of atopy patch test for diagnosis of food allergy-related gastrointestinal symptoms in children. Pediatr Allergy Immunol. 2015;26:737-41
20. Edwards KP, Martinez BA. Atopy patch testing for foods: a review of the literature. Allergy Asthma Proc 2014;35:435-43.
21. Greer FR, Sicherer SH, Burks AW et al; American Academy of Pediatrics Committee on Nutrition; American Academy of Pediatrics Section on Allergy and Immunology. Effects of early nutritional interventions on the development of atopic disease in infants and children: the role of maternal dietary restriction, breastfeeding, timing of introduction of complementary foods, and hydrolyzed formulas.Pediatrics. 2008;121:183-91
22. Muraro A, Halken S, Arshad SH, et al; EAACI Food Allergy and Anaphylaxis Guidelines Group. EAACI food allergy and anaphylaxis guidelines. Primary prevention of food allergy. Allergy. 2014;69:590-601
23. Boyce JA, Assa’ad A, Burks AW, et al. Guidelines for the diagnosis and management of food allergy in the United States: summary of the NIAID-sponsored expert panel report. J Allergy Clin Immunol. 2010;126(6 Suppl):S1-58
24. Fiocchi A, Pawankar R, Cuello-Garcia C, et al. World Allergy Organization-McMaster University Guidelines for Allergic Disease Prevention (GLAD-P): Probiotics. World Allergy Organ J. 2015; 8:4
25. Boyce JA, Assa’ad A, Burks AW, et al. Guidelines for the diagnosis and management of food allergy in the United States: summary of the NIAID-sponsored expert panel report. J Allergy Clin Immunol. 2010;126(6 Suppl):S1-58
26. Boyle RJ, Ierodiakonou D, Khan T, et al. Hydrolysed formula and risk of allergic or autoimmune disease: systematic review and meta-analysis. BMJ. 2016;352:i974
27. Fiocchi A, Assa’ad A, Bahna S; Adverse Reactions to Foods Committee; American College of Allergy, Asthma and Immunology. Food allergy and the introduction of solid foods to infants: a consensus document. Adverse Reactions to Foods Committee, American College of Allergy, Asthma and Immunology. Ann Allergy Asthma Immunol. 2006;97:10-20
28. Du Toit G, Roberts G, Sayre PH, et al; LEAP Study Team. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med. 2015;372:803-13
29. Togias A, Cooper SF, Acebal ML, et al. Addendum guidelines for the prevention of peanut allergy in the United States. Report of the NIAID-sponsored expert panel. Allergy Asthma Clin Immunol. 2017;13:1
30. Houben G, Burney P, Chan CH, Crevel R, Dubois A, et al. Prioritisation of allergenic foods with respect to public health relevance: Report from an ILSI Europe Food Allergy Task Force Expert Group. Food Chem Toxicol 2016;89:8-18
31. Nurmatov U, Dhami S, Arasi S, et al. Allergen immunotherapy for IgE-mediated food allergy: a systematic review and meta-analysis. Allergy. 2017 Jan 6. [Epub ahead of print]
32. Peters RL, Allen KJ, Dharmage SC,et al. Natural history of peanut allergy and predictors of resolution in the first 4 years of life: A population-based assessment. J Allergy Clin Immunol. 2015;135:1257-66
33. Pite H, Prates S, Borrego LM, et al. Resolution of IgE-mediated fish allergy. Allergol Immunopathol (Madr). 2012;40:195-7
34. Kokkonen J, Tikkanen S, Savilahti R: Residual intestinal disease after milk allergy in infancy. J Pediatr Gastroenterol Nutr 2001; 32: 156-61.
Committed to Finding the Cause of Your Allergy & Treating it Where Allergy Patients come to Get Well
EGGS
1. Sausage and meatloaf unless ground at home and prepared with no egg.
EGGS are to be avoided in ANY form. This is a list of foods where eggs commonly occur. If there is any question regarding a prepared food, investigate the contents listed on the label. EGG OR EGG IN ANY OTHER FORM OF EGG WHITE OR YOLK, INCLUDING POWDERED.
2. Cooked or raw eggs, soufflés, fritters and egg noodles.
3. Cake, cookies, doughnuts, macaroons, pastries, batters (pancakes and waffles), pretzels, French toast. Pie crust, muffins, meringues,
4. Ice cream, water ices and sherbets unless made at home from an egg free powder.
5. Mayonnaise, hollandaise sauce, tartar sauce, salad dressing with egg, icings, marshmallows, nougats, fondants, chocolate creams, filled candy bars, etc.
6. Ovaltine, ovomalt and root-beer.
7. Prepared flours such as Bisquick, pancake flour, etc.
8. Baking powder except Royal and K.C.
CORN
Corn and maize products occur in a large variety of foods. The ubiquitous use contributes to repetitious ingestion thereby making it one of the most common allergic foods, and one most difficult to eliminate from one’s diet.
Corn may cause allergic symptoms as a contactant (talcs, bath oils and powders, starched clothing and corn adhesives) as an inhalant (fumes from vegetable forms of corn as they cook) and as an ingestant (as corn and corn products are eaten)
COMMON SOURCES OF CORN
Alcoholic Beverages & vinegars:
All ale, beer, brandy, gin whiskies, and vodka when manufactured in the USA are usually fortified with corn, Most domestic wines contain corn except for California wines of 13% alcoholic content or less, California sparkling wines, and California wines above 13% alcohol are allowed to be fortified with corn, imported wines and brandies are usually corn free. White or acetic acid vinegar is usually derived from corn and is used commercially for salad dressings, pickles, sauerkraut, and sauces.
Corn Meal:
Buckwheat, oatmeal or corn meal is scattered on the hearth before baking panless loaves of bread. This layer may be removed by cutting by quarter of an inch off the bottom of the loaf. Do not scrape it off. Corn meal is also used in cereals, scrapple, mush, Johnny cake, indian pudding, and other recipes, as well as the batter for deep frying foods.
Corn Oil:
Corn oil is comparatively inexpensive and occurs in grease for deep fat frying and oil salad dressings.
Corn Starch:
Corn starch is used as a thickening agent in gravies, icings and frosting, pies, sauces, white sauce and many other items. Many baking powders contain cornstarch. Most tablets, pills and capsules contain cornstarch as a filler. Starched clothing and beddings, and adhesives in shoes may cause contact symptoms. Cornstarch is also dusted on many brands of paper cups and plates, waxes and plastic containers, and plastic bags to prevent foods from sticking to them. There are aerosol starch preparations for laundry use in the home. When sprayed, these preparations would be inhaled as well as contacting the skin.
Corn Sugars (Dextrose & Glucose):
These sugars are derivatives of corn starch. Corn sugar does not become sticky and imparts a smooth texture to candies. It is used in nearly all commercial chocolates and caramels, cough drops, hard candies, lozenges, and suckers. The malted preparations used in ice cream, candies, and cereals are derived from corn and wheat. Most bacon, canned fruits, ham, ice cream, jello, jams, preserves, processed cheese, and soft drinks contain corn sugar. Corn sugar is the most common sugar used for intravenous feeding. Synthetic vitamin C, citric acid of commerce, Sorbitol, and Mannitol are derived from corn sugar. Corn dextrins and adhesives are used on stamps, envelopes and many other products. Some cigarettes are blended with corn sugar.
Vegetable oils are not required to be identified on commercial labels so one must assume that commercial products containing oils will include some amount of inexpensive corn oil. Sugars also do not have to be designated as being corn, cane or beet for labeling purposes. This requires, then , avoidance of all commercially sweetened products in order to totally eliminate corn from one’s diet.
Always read labels. When inquiring whether a product contains corn, ask about each item by its individual name under the ripe corn list. For example, when checking a bakery product, ask if the product contains any corn flour, corn meal, corn starch, corn oil (Mazola), corn sugar (dextrose), or corn syrup. Do not accept the word of untrained personnel unless you inventory your inquiry by every specific name of ripe forms of corn.
The following is a list of products which may contain corn. Corn-free brands of canned goods, baked goods, frozen foods, jams, etc, can be found. Ripe forms of corn are corn meal, corn oil, corn starch, corn sugars, corn syrups, grits, or popped corn.
FOODS CONTAINING CORN AND OTHER CORN CONTACTS
Adhesives | Gravies | Pastries |
Envelopes | Grits | Peanuts butters (unless 100% natural) |
Stamps | Gums, chewing | Plastic food wrappers (the inner surfaces may be coated with corn starch) |
Stickers | Gin | Preserves |
Tapes | Ham | Puddings |
Artificial sweeteners | Cured | Rice |
Aspirin & other tablets | Tenderized | Coated, instant |
Bascon | Harvard beets | Salt cellars in restaurants |
Baking mixes | Hominy | Salad dressing |
Biscults | Ices | Sandwich spreads |
Pie crusts | Ice creams | Sauces for |
Doughnuts | Inhalants | Sundaes |
Pancake mixes | Bath powders | Meats |
Baking powders | Cooking fumes of fresh corn pop corn | Fish |
Batter for frying | Pop corn | Vegetables |
Beverages, carbonated | Starch | Sausages, cooked or table ready |
Bleached wheat flours | Starch while ironing starch clothing | Sherbets |
Breads and pastries | Talcum’s | Soups |
Cakes | Jams | Creamed |
Candy | Jellies | Thickened |
Candy bars | “jello” | Vegetable |
Commercial candies | Leavening agents | Sugar powdered |
Box candies, all grades | Baking powders | Syrups, commercially prepared |
Catsups | Yeast | Talcum’s |
Cereals-commercial | Liquors | Teas, instant |
Cheeses | Ale | Tooth paste |
Coffee-instant | Beer | Tortillas |
Cookies | Gin | Wines, American |
Confectioner’s sugar | Whiskey | Vegetable, frozen |
Cough syrups | Meats | Vitamins |
Cream pies | Bacon | “Scotch” & bourbon |
Cream puffs | Bologna | Vanillin |
Cups, paper | Cooked, with gravies | Vinegar, distilled |
Dates, confection | Ham, cured or tenderized | Whiskies |
Dentifrices | Lunch ham | Scotch” & Bourbon |
Excipients or diluents in | Sausages, cooked | American brandies, both apple and grape |
Capsules | Wieners (Frankfurters) | Wines, american |
Lozenges | Milk, in paper cartons | Dessert |
Ointments | Mono-sodium glutamate | Sparkling |
Suppositories | Oleomargarine | Salt |
Tablets | Paper containers | Fortified |
Vitamins | Boxes |
|
Flour, bleached | Cups |
|
French dressing | Plates-these 3 only when foods have a moist phase in contact with these cartons |
|
Frostings |
|
|
Fruits |
|
|
Fortified |
|
|
Canned |
|
|
Frozen |
|
|
Gelatin capsules |
|
|
Gelatin desserts |
|
|
Glucose products |
|
|
Graham crackers |
|
|
Grape juice |
|
|
|
|
|
MILK
Milk is to be avoided in ANY form. This is a list of foods where milk commonly occurs. If there is any question regarding a prepared food, investigate the contents listed on the label.
Milk is widely used in processed, packaged foods. It can be referred to by many different names. Therefore, AVOID all food products with a label that states MILK, DRY MILK Solids, Nonfat Milk Solids, Buttermilk, Cream, Whey, Yogurt, Cheese, Curds, Butter, Margarine (can contain milk), Sour Cream, Casein, Casein ate, Sodium Casein ate, Lactalbumin, Lactose.
1. Custard, junket, ice cream, milk pudding
2. Batters, waffles, pancakes, cake, cookies and prepared flours (such as Bisquick)
3. Ordinary bread
4. Malted milk, oval tine, coco malt, drinking chocolate, buttermilk, canned or dried milk
5. Milk chocolate candy, chocolate creams, filled candy bars nougat
6. Cottage cheese and other cheese
7. Any foods prepared with milk, cheese or cream, such as gravies, cream sauces, fritters, rarebits, timbales, soufflés, soufflés, au gratin dishes, omelets
8. Frankfurters and other sausages (dried skin milk used as binder) and wiener schnitzel
9. Powdered milk
Soy
Soybeans have been grown in Asia for centuries, especially in China, where they have provided the bread, protein and oil. Since the beginning of the 19th century, American farmers have grown soybeans for livestock, feed or for fertilizer.
Chemists have also found many uses for soybeans, which are proving to be a bonanza. Ford Motor Company uses them to make plastic window frames, steering wheel, gearshift knobs, distributor, upholstery fabric, and other parts. Rubber substitutes and lecithin in leaded gasoline are also made from soybeans.
Many new food and industrial uses of soy can be expected. If you remember that soybeans are used as flour, oil, milk, nuts and meat extenders, it will be possible to anticipate most new food contacts. When purchasing prepared foods, consider soy as a possible ingredient if the label says vegetable oil, vegetable broth or textured vegetable protein.
Eating in restaurants almost always means a soy exposure, as most restaurants and fast-food chains cook with soy oil or flour. Soybean flour containing only one percent oil is now used by many bakers in dough mixtures for breads, cakes, rolls, and pastries, to keep them moist and fresh several days longer. The roasted beans are often used in place of peanuts on breakfast rolls. Some biscuits and several crisps crackers also contain soybean flour.
FOOD SOURCES OF SOY
Artificial meats and nuts | Miso | Fertilizer |
Baby foods | Natto | Fish food |
Bakery goods | Tempeh | Fodder |
Cake mixes (May contain artificial fruit made from soy) | Tuna (Packed in vegetabe oil) | Glycerine |
Candies | Margarine or oil on vegetables soy sprouts | Illuminating oil |
Caramels | Other Sources: | Lecithin |
Carob chips | Adhesives | Linoleum |
Chocolate chips | Automobile parts | Lubricating oil |
Hard candies | Blankets | Make-up |
Nuts candies (Lecithin, derived from soy, is used in candies to prevent drying and to emulsify fats) | Candies | Massage cream |
Cereals | Tortilla chips | Nitroglycerine |
Fried products | Ice cream (diary and tofu) Margarine and butter substitutes | Paints |
Corn chips | Meats | Paper finishes |
Potato chips | Canned meats and fish Hamburgers (fast food) | Paper finishes |
Pastas: | Luncheon meats | Paper sizing |
Macaroni | Pork-link sausages | Printing ink |
Noodles | Milk substitutes | Soap |
Spaghetti | Infant formulas | Telephones |
Peanuts butter (some) | Non-dairy creamers | Textile finishing’s |
Processed cheeses (some) | Soy milk | Toys |
Salad dressing (may contain soy oil, but list only vegetable oil on the label) | Nuts: Any roasted in soy oil Soy (formed to look like other nuts) Soybeans (toasted, salted and used as nuts oils (Crisco, Spry solid or liquid) | Varnish |
Sauces | Celluloid | Vitamins |
Lea & parries | Cloth |
|
Soy sauce | Clothing |
|
Steak sauce | Coffee substitute |
|
Tamari | Cosmetics |
|
Teriyaki sauce | Custard |
|
Worcestershire sauce | Diet aids |
|
Soup (may contain soy oil and/or lecithin) | Dog foods |
|
Tofu | Enamels |
|
Wheat-Free Diet Food you Cannot have:
BEVERAGES:
Coffee substitutes and other beverages made from wheat products. (Check labels for ingredients.) Malted drink, beer and ale.
BREADS:
Whole wheat, graham, gluten and white breads, rolls, muffins and biscuits. Doughnuts, popovers, sweet rolls, Johnny cake, pancakes, waffles, rusks, pretzels, zwieback and cracker (except Ry-krisp). Prepared mixes for pancakes, waffles, biscuits, muffins, doughnuts, breads and rolls. Rice, potato and soybean breads, rolls, muffins and biscuits; corn and rye breads, rolls and muffins unless made at home without wheat flour.
BREADED FOODS:
In which breading mixture contains wheat products.
CEREALS:
Wheat cereals and those containing wheat or wheat products. (Real labels carefully)
DESSERTS:
Cakes, doughnuts, dumplings, pastries, commercial sherbets, ice creams cones. Custards, cookies, pies and puddings made with wheat products. Prepared mixes for cakes, cookies, ice cream, pudding and pie crusts, unless the list of ingredients on the label shows no wheat products.
MEAT, POULTRY, GAME, FISH AND SEAFOOD:
Swiss steak. Bread and cracker stuffing’s. Chili con carne, croquettes, fish or meat patties and loaves, unless made at home without wheat products (See recipes.) (Commercially and dealer-prepared meats frequently contain wheat products.)
MISCELLANEOUS:
Malt products. Dumplings, noodles, spaghetti, macaroni, ravioli, mostaccioli, vermicelli, soup rings, alphabets and kindred products.
SALAD DRESSINGS:
Any salad dressing thickened with wheat flour.
SAUCES AND GRAVIES:
Gravies, butter sauces, cream and white sauces unless homemade without wheat flour. Read labels on commercial sauces and do not use if they contain wheat products.
SOUPS:
Cream, unless made at home without wheat flour. Vegetable and meat soup, chowders and bisques if thickened with wheat products.
SWEETS:
Commercial candies that contain wheat products. Read labels.
VEGETABLES:
Any vegetable prepared or served with a sauce thickened with wheat flour or those prepared and served in any way with wheat products.
Wheat and wheat products include1) all the following flours: white, bread, all-purpose, cake, pastry, self rising, wheat whole wheat, entire wheat, cracked wheat, graham, enriched, durum, phosphate; (2) also: wheat, wheat germ, bran farina, semolina, (3) and in addition, cracker, cracker meal, bread crumbs and malt.
NOTE: When you buy packaged foods read the labels carefully to be sure the list of ingredients includes none of the above. When you purchase food lacking a list of ingredients and when you eat away from home, if in doubt about any food and accurate information cannot be secured, substitute a choice about which there can be no doubt.
COMMON SOURCES OF YEAST
I. The following foods contain yeast as an additive ingredient in preparation (often called leaving).
BREADS CANNED ECE BOX BISCUITS: COOKIES
CAKE & CAKE MIXES Burdens, Pillsbury & General Mills
CRACKERS
FLOUR, Enriched with vitamins form yeast : General Mills, Inc.
Flour corporation flour and enrichment products,
Pfizer Laboratories enrichment product, Hungarian Flour Mills
HAMBURGER BUNS PASTRIES
HOT DOG BUNS PRETZELS
MILK, fortified with vitamins ROLLS, homemade or canned
MEAT, FISH or FOWL, fried in cracker crumbs
SALT RISING BREAD
II. The following substances contains yeast or yeas-like substances
Because of their nature or nature of their manufacture
or preparation.
BLACK TEA MUSHROOMS SOY SAUCE
BUTTERMILK SOUR CREAM TRUFFLES
CHEESE OF ALL KINDS, including COTTAGE CHEESE
CITRIC ACID- almost always a yeast derivative
CITRUS FRUIT JUICES, of all types, whether frozen or
canned-only home squeezed are yeast-free
DRIED FRUITS, of all types (prunes, raisins, dates, etc.)
FERMENTED BEVERAGES OF ALL TYPES: Beer, brandy,
gin, rum, whisky, wine, vodka, root beer, ginger ale.
MALTED PRODUCTS OF ALL TYPES: Cereals, candy or milk
Drinks, which have been malted
MONOSODIUM GLUTAMATE, may be a yeast derivative
VINEGARS of all types: apple, pear, grape and distilled¬¬¬¬—these
may be used as such or they will be used in the following foods: all
baby cereals, Bar B-Q sauce, catsup, condiments, chili and
peppers, etc. French dressing, horse-radish, mayonnaise, mince pie,
olives, pickles, salad dressing, sauerkraut, tomato sauce.
III. The following contain substance that are derived from yeast or have
Their source from yeast.
ANTIBIOTICS: B-12, Chloromycetin, Lincocin, mycin drugs,
Penicillin, Tetracyclines, and any others derived from mold cultures
Multiple vitamin capsules or tablets with vitamin “B: made from
Yeast.
Vitamin “B” capsules or tablets if made from yeast
U.S. vitamin products
Citric acid
Endo’s vitamin products
Laxo-Funk
Lilly’s vitamin products which contain vitamin B-12
Lederle’s vitamin products
Manibee tablets, S.C.T
Massengill vitamins
Mead Johnson’s vitamin which contain B-12
Parke Davis’s vitamin product: VIBEX
Phoscaron-D
Squibbe vitamin product if indicated on label
Vi-Litron Drops
Dormison rest capsules
Zylax, Zymelose, Zymenol
Be sure to read labels. Additions may be found to this list.
COCONUT ALLERGY
Contact dermatitis to coconut is more common than food allergy.
Coconut derived products (such as coconut diethanolamide, cocamide sulphate, cocamide DEA, CDEA) can cause contact allergic dermatitis, presents in cosmetics including some hair shampoos, moisturizers, soaps, cleansers, and hand washing liquid. As with any contact dermatitis, an itch blistering rash may arise a day or two after contact with the allergen, and take several days to resolve, if contact dermatitis or ingestive allergy to coconuts products is suspected, then patch testing or provocative neutralization testing are the appropriate methods for diagnosis.
COMMON SOURCES OF COCONUT
Cakes/Pies | Fried Foods |
Chocolates | Crackers |
Candies | Desserts |
Infant Formula | Whipped Topping |
Curries | Non-Dairy Creamer |
Laksa | Asian soups & meals (especially Thai) |
Processed Foods | Cosmetics |
Shampoos | Moisturizers |
Bar Soaps | Cleansers |
Hand Washing Liquids | Suntan Lotions |